Sleep is fundamental to all life. Without it, the consequences to our physical, psychological, and emotional health are significant.
In the short-term, a lack of good quality sleep can impact our day-to-day performance. In contrast, a consistent pattern of sleep problems has been associated with the development or worsening of a variety of illnesses.
Over the last 50 years, research has attempted to understand the associations between sleep, health, and well-being. Only recently are we starting to untangle these relationships.
From what we have discovered, not only is the amount of restorative sleep we get essential, but so is getting consolidated amounts of each stage of sleep, especially Rapid Eye Movement Sleep (REM) and Slow Wave Sleep.
To further understand how sleep impacts health, we first need to explore the different stages of sleep and the purpose of each.
Get Your FREE Sleep Guide
- Learn how to naturally improve your sleep
- Dietary recommendations, supplements, and lifestyle changes
- Developed exclusively by our medical doctor
Stages of sleep
Sleep is characterized by two distinct states – REM sleep and non-Rapid Eye Movement Sleep (NREM sleep). How these are differentiated is through studying:
- the amplitude (depth) and frequency (speed) of brain wave activity
- levels of muscle tension
- changes in eye movements and heart rate (see Figure 1).
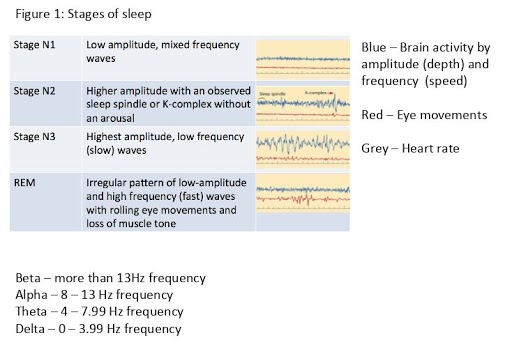
As we can see, brain wave activity is the best indicator of the different stages of NREM.
In contrast, REM looks similar to a waking, relaxed state. This is the main reason that muscle tension, eye movements, and heart rate are examined during sleep – to differentiate REM from wakefulness.
Until recently, Non-REM sleep was further broken down into four stages (Stages 1, 2, 3, and 4). Now, Stages 3 and 4 are combined into one category, leaving us with N1, N2, and N3 (Iber et al, 2007).
N1
Broadly in the context of adults, when we get into bed, activity in our brain starts to slow, and we enter N1. N1 is officially classified as the first stage of being asleep, but it is not always distinguishable from a relaxed but awake state. As such, we also look for rhythmic slow rolling eye movements. The first period of N1 should last a few minutes (1-10 minutes) before the transition to N2 occurs.
N2
The onset of N2 is defined based on an observed K complex ( a brief but huge surge in brain activity – without arousal), or sleep spindle (a rapid but short burst of high-frequency brain waves). This first period of N2 should last approximately 10-25 minutes. As we might expect, we then transition from N2 to N3.
N3
After approximately 20-40 minutes of N3, we should then go back into N2, albeit briefly (5-10 minutes), before entering our first REM period, which is very short (1-5 minutes). Although this pattern is repeated throughout the night, the first ‘sleep cycle’ is generally shorter at 70-100 minutes. The following sleep cycles are roughly 90-120 minutes long.
Overall, REM should take up between 20-25% of an adult’s typical night and NREM the rest. However, the dynamics of both REM and NREM (specifically N3) change throughout the night. The first third of the night is characterized by longer consolidated blocks of N3 and minimal amounts of REM, while the opposite is observed during the last third of the night.
Sleep spindles
N1 is mostly thought to be a ‘gateway’ to sleep; however, our understanding of the intention of N2 has changed over time. It is now believed that sleep spindles may be associated with learning and memory through reactivation of the experiences and things learned throughout the day.
Spindles play an essential role in both sensory processing and long term memory consolidation because they are generated in the TRN. During sleep, these spindles are seen in the brain as a burst of activity immediately following muscle twitching.
Where REM has traditionally been associated with consolidating memory and, of course, dreaming, it is now considered central to the regulation of our emotions as well. This includes extinguishing the negative impact of traumatic and stressful events.
What is deep sleep?
Together, Stages 3 and 4 (or more recently, N3) is also known as Slow Wave Sleep (SWS) or the deep sleep stage.
N3 is defined based on 20% (or more) delta activity within a 30-second block of sleep (epoch). In addition to being defined as N3, SWS, and deep sleep, this period is also often referred to as Delta Sleep.
Due to the depth of SWS, being awoken during this period is difficult and likely to result in feelings of grogginess and disorientation, known as sleep inertia (Tassi & Muzet, 2000).
Within sleep depth, we can also characterize Slow Wave Activity (SWA), which is defined based on very slow Delta waves (0.5-2.0Hz) with high peak-to-peak amplitudes (>75µV – microvolts).
Levels of SWA not only reflect sleep intensity; it is also widely accepted that they are a marker of our sleep drive (Greene & Frank, 2010).

What are the benefits of deep sleep?
The benefits of SWS can be seen in terms of both our physical health and our ability to learn and remember (Leger et al, 2018). One of the main hormones associated with SWS is the production of Growth Hormone (GH).
Production of hormones
For men, GH is intimately tied to SWS, with pulses in GH being produced during each period of SWS, whereas women make GH throughout the 24-hour cycle. Still, increased pulses are generally observed during the first cycle of SWS.
While GH is, as we can imagine, good for development during childhood and early adulthood, in later adulthood, GH helps us recover physically by promoting the repair of damaged tissue and reducing oxidative stress that builds up in the muscles.
Other hormones modulated during SWS include Thyroid-stimulating hormone (TSH), prolactin, ghrelin, and cortisol. This indicates the role for SWS across several other health domains including fertility, stress responsivity, and appetite regulation.
Blood sugar regulation
Moreover, studies where an individual is deprived exclusively of SWS demonstrate a significant role for SWS in glucose regulation and insulin sensitivity. This suggests a role for SWS, or a lack of it, in developing Type II Diabetes (Tasali et al, 2008).
Enhances immune system
There is also an interesting relationship between SWS and immunity. Anti-inflammatory cytokines have been to suppress SWS and pro-inflammatory cytokines, thereby enhancing SWS. This is one reason why when we don’t feel very well, we want to go to sleep.
May prevent Alzheimer’s
Finally, one of the more recent findings is that we clear a particular toxin (Beta Amyloid) from the brain during SWS (Varga et al, 2016). High levels of this toxin in the brain have been associated with Alzheimer’s Disease, so enhancing SWS has been suggested as a preventative measure (Wunderlin et al, 2020).
Our understanding of the role of SWS in learning and memory has mainly come from split-night studies where individuals are either prevented from sleeping in the early part of the night (a period rich in SWS) or the early hours of the morning (a period rich in REM).
From these studies, it appears that there is an association between SWS and some types of memory consolidation.
What happens when you don’t get enough deep sleep?
If we think about the number of biological systems regulated during SWS, going without it for too long is likely to have a significant impact on our health and well-being.
Certainly, several short-term experiments whereby SWS has either been reduced or eliminated demonstrate reductions in pain thresholds and increases in fatigue levels. That said, our bodies have an amazing capacity for attempting to manage a short period of reduced SWS.
If we are deprived of a good sleep for a night, SWS predominates during the following night, and in particular, the amount of SWA significantly increases.
In the longer-term associations between reduced SWS and several diseases and illnesses have been observed, most notably, in an increased risk for hypertension (high blood pressure).
Sleep disorders and deep sleep
Several sleep disorders are associated with reduced amounts of SWS, most notably:
- Restless Legs Syndrome (itchy crawly sensations in the legs which get worse in the evening and are alleviated, albeit temporarily, by moving around).
- Periodic Limb Movement Disorder (twitches in the legs, usually, during fragmented sleep).
- Obstructive Sleep Apnoea (partial or complete closure of the airway during sleep which also fragments sleep).
How much deep sleep do you need?
Interestingly, unlike the other sleep stages, pronounced differences have been observed in terms of sex and age in the amount of deep sleep we need.
For example, women achieve more SWS than men, and the amount of SWS we achieve decreases every decade following puberty for both sexes (Ohayon, 2004).
The National Sleep Foundations’ recommendations on sleep quality suggest 20-25% of a school-aged child and/or teenagers’ sleep should comprise of SWS; for adults, this may be between 16-20%.
Further, due to individual variability in SWS, there is no recommendation for the amount older adults need, but it is common to see less than 10% in those over 70.
How to get more deep sleep?
Given the capacity for SWS to self-regulate, the best way to get the right amount of SWS is to give yourself enough time to sleep.
- That said, there are a few studies that demonstrate that exercise increases the amount of SWS you get at night.
- Some medications have also been associated with increased SWS, such as antidepressants and pain relief medications (Walsh, 2009). Conversely, some sleep medications have been associated with reduced levels of SWS, in particular, Benzodiazepines (Petrovic et al, 2003).
- Whilst techniques such as transcranial magnetic stimulation and transcranial direct-current stimulation (tDCS) have been explored, the results have been very mixed (Underwood, 2016).
- More recently, acoustic sensory stimulation has been used in this context with promising results.
The main thing to note is that many of these studies that use pharmacological and non-pharmacological strategies to increase SWS have either created an SWS debt through sleep deprivation prior to the strategy being implemented or not accounted for how much SWS debt the individual had prior to the method being employed.
As such, it may be that the increases in SWS observed using these methods may be compensating for an existing sleep debt and that an individual cannot obtain SWS above their personal optimal threshold at that time (Ferra et al, 1999).
Conclusion
Although all sleep stages have essential functions, SWS is the sleep stage that is most vital to physical health.
While the impact of reduced SWS on our day-to-day functioning is undeniable, there is still much work to be done to examine the long-term effect of reduced SWS on health outcomes.
That said, there is clearly a role for SWS in the development of some illnesses. This has led to the development of several strategies designed to increase levels of either SWA or SWS.
While many are still in their infancy, the results have not always been consistent or are impractical at present, except for exercise. There is, however, one main thing you can do to get SWS, and that is to prioritize a good night’s sleep.
Explore More








