- Q: What is Prostatitis?
- Q: What are the Different Types of Prostatitis?
- Q: What are the Symptoms of Prostatitis?
- Q: What Causes Prostatitis?
- Q: What are the Risk Factors for Developing Prostatitis?
- Q: How to Diagnose Prostatitis?
- Q: Can You Explain the Difference Between Prostatitis and BPH?
- Q: Does Prostatitis Increase the Risk of Prostate Cancer?
- Q: Does Prostatitis Go Away on Its Own?
- Q: How to Treat Prostatitis?
- Q: What Natural Treatments Are Available for Prostatitis?
- Key FAQs on How to Cure Prostatitis
- Q: What's Your Concluding Advice for Men Dealing with Prostatitis?
- Our Medical Review Process
- Our Editorial Guidelines
- Medical Disclaimer
- Source
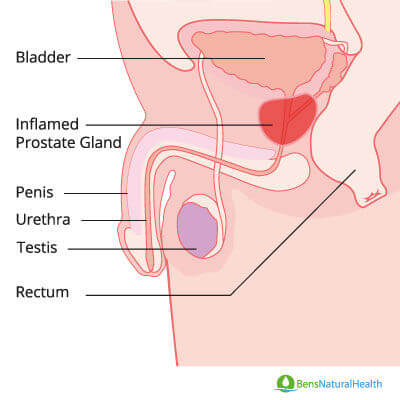
If you’ve been experiencing discomfort, pain while urinating, or other urinary issues, you might be wondering if prostatitis is the cause. But what is prostatitis?
Prostatitis refers to inflammation of the prostate gland, which can stem from bacterial infections or other underlying conditions. Unlike an enlarged prostate (benign prostatic hyperplasia, or BPH) or prostate cancer, prostatitis has distinct causes and symptoms that require targeted treatments.
We spoke with Dr. Hamad Shafqat, a leading urologist specializing in prostate health, to understand the different types of prostatitis, their causes, symptoms, and the best treatment approaches. Dr. Shafqat shared valuable insights, evidence-based recommendations, and expert guidance on managing prostatitis effectively.
Dr. Shafqat has also provided research-backed information for this article to help you gain a deeper understanding of prostatitis and its management.
Q: What is Prostatitis?
Dr. Shafqat answers: Prostatitis is a term we use in medicine to describe a set of symptoms caused by infection or inflammation of the prostate gland. It’s important to understand that this condition is distinct from other prostate conditions like benign prostatic hyperplasia (BPH), which involves an increase in prostate cells, or prostate cancer, where malignant cells form and multiply.
The nature of prostatitis is quite complex, and the symptoms can vary significantly depending on the cause and type. This is why it’s essential for us as medical professionals to identify the underlying cause to provide effective treatment accurately.
Q: What are the Different Types of Prostatitis?
Dr. Shafqat answers: Prostatitis isn’t a single condition; rather, it’s a broad term that describes inflammation of the prostate gland. There are four main types, each with its own causes and symptoms.
Acute Prostatitis
Acute prostatitis is a rare but severe form of prostatitis caused by a bacterial infection. Symptoms develop rapidly and can include:
- High fever (above 38°C)
- Intense pelvic pain
- Some experience frequent night-time urination (nocturia) and find it painful to urinate.
- Muscle aches
- Pain in the scrotum, penis, thighs, and lower back
- Acute urinary retention in about 10% of cases, requiring catheterization
Bacteria from the bowel or bloodstream can infect the prostate, leading to this condition. It can also be caused by sexually transmitted diseases and inflammatory conditions in the urinary tract. Treatment typically involves antibiotics, and in severe cases, catheterization may be necessary to drain urine.
Chronic Bacterial Prostatitis
This condition involves a persistent bacterial infection that lasts at least three months. It tends to cause flare-ups, leading to recurring urinary tract infections (UTIs). Symptoms include:
- Frequent urination, especially at night
- Pelvic discomfort
- Pain in the lower back
- Discomfort during ejaculation
Since bacteria cause chronic bacterial prostatitis, long-term antibiotic treatment is required. Completing the full course of antibiotics is essential to prevent microbial resistance. According to research, in some cases, resistance to treatment may indicate the presence of a prostatic abscess.
Chronic Non-Bacterial Prostatitis (Chronic Pelvic Pain Syndrome – CP/CPPS)
This is the most common form, affecting 9 out of 10 men with prostatitis. Unlike bacterial prostatitis, this type isn’t caused by a bacterial infection and doesn’t respond to antibiotics. Symptoms include:
- Persistent pelvic pain
- Painful and frequent urination
- Discomfort in the perineum, testicles, or lower back
- Pain during or after ejaculation
As the research shows, diagnosing chronic prostatitis requires ruling out bacterial causes through urine and medical history analysis. Treatment focuses on symptom management through medications, physiotherapy, and lifestyle changes. Some cases may be linked to irritable bowel syndrome (IBS), chronic fatigue syndrome, and nerve dysfunction.
Asymptomatic Prostatitis
Asymptomatic prostatitis is an interesting type because, as the name suggests, it doesn’t present any noticeable symptoms. We usually discover it incidentally while testing for other conditions, such as prostate cancer. While patients may not experience symptoms, we often find elevated PSA levels and white blood cells or pus cells in their urine. In fact, about one-third of men with elevated PSA levels have asymptomatic prostatitis.
Get Your FREE PSA Lowering Diet Plan!
- Naturally lower PSA levels
- Reduce nighttime trips to the bathroom
- Enjoy better bladder control and urine flow
Q: What are the Symptoms of Prostatitis?
Dr. Shafqat answers: Prostatitis can affect men of any age, but we see it most commonly in younger and middle-aged men, typically between 30 and 50 years old. As the research confirms, For men over 50, it’s actually the third most common urinary tract issue.
As the study shows, prostatitis accounts for about two million visits to health care providers in the United States each year.
The severity of symptoms varies depending on the type, but here are the most common symptoms to watch for:
- Painful urination
- Frequent urination, especially at night (nocturia)
- Blood in the urine or cloudy urine
- Pain in the abdomen, groin, or lower back
- Discomfort in the perineum (the area between the scrotum and rectum)
- Pain in the penis or testicles
- Flu-like symptoms (fever, chills, body aches)
- Painful ejaculation or sexual dysfunction
- Urethral discharge
If you’re experiencing these symptoms, it’s essential to consult a healthcare provider for proper diagnosis and treatment.
Q: What Causes Prostatitis?
Dr. Shafqat answers: If you are wondering what is the most common cause of prostatitis, you should know that the causes of prostatitis depend on the type:
- Acute Prostatitis: Caused by bacteria, often from a UTI or sexually transmitted disease (STD). According to the study, it may also occur after a prostate biopsy or prolonged catheter use.
- Chronic Bacterial Prostatitis: Persistent bacterial infections that often stem from incomplete antibiotic treatment or antibiotic-resistant bacteria.
- Chronic Non-Bacterial Prostatitis (CP/CPPS): The exact cause is unclear, but possible triggers include urine reflux into the prostate, nerve dysfunction, stress, or a history of UTIs. There is also some research indicating that CPPS may be linked to and triggered by other conditions such as stress, irritable bowel syndrome (IBS), and chronic fatigue syndrome.
- Asymptomatic Prostatitis: The exact cause of asymptomatic inflammatory prostatitis is not known. The research team looked at the semen of 37 men with asymptomatic prostatitis and found that the semen had about eight different types of bacteria. The bacterial count was also related to the high white blood cell count.
Q: What are the Risk Factors for Developing Prostatitis?
Dr. Shafqat answers: Several factors can increase your risk of developing prostatitis, particularly those that increase your susceptibility to UTIs and STDs. These include:
- Insufficient fluid intake
- Urinary catheter use
- Having multiple sexual partners
- Engaging in unprotected vaginal or anal intercourse
- Advanced age
- Recurring UTIs
- Previous episodes of prostatitis
- Genetic predisposition
- Pelvic injuries
- Inflamed testicles
- HIV/AIDS infection
- Stress and mental distress

Q: How to Diagnose Prostatitis?
Dr. Shafqat answers: Are you wondering how to test for prostatitis? We use several diagnostic tools and tests to confirm prostatitis:
- Urine Test: This is particularly helpful for diagnosing bacterial prostatitis. We look for bacteria and excessive white blood cells in the urine.
- Blood PSA Test: Most men with acute prostatitis show a significant increase in PSA levels. While this elevation is typically due to inflammation, we use this test along with other examinations to help confirm the diagnosis.
- Digital Rectal Exam (DRE): As a urologist, I perform this examination to check if the prostate is enlarged, swollen, or tender. This also helps rule out other serious prostate conditions.
- Urodynamic Tests: We measure post-void residual urine to assess bladder emptying capabilities. This is important because urinary retention can lead to prostate infection if the urine contains bacteria. Incomplete bladder emptying can also cause recurrent urinary tract infections.
- The UPOINT System: This is a clinical profiling system we use to categorize symptoms into six categories for more personalized treatment. These categories include:
- Urinary signs
- Psychological dysfunction
- Organ-specific symptoms
- Infectious causes
- Neurological dysfunction
- Tenderness of pelvic floor muscles
This system has been validated through multiple clinical trials and is becoming increasingly widespread in practice.

Q: Can You Explain the Difference Between Prostatitis and BPH?
Dr. Shafqat answers: While BPH (Benign Prostatic Hyperplasia) and prostatitis can cause similar urinary symptoms, they’re actually two distinct conditions. BPH involves an enlargement of the prostate due to the growth of prostate cells, which eventually compresses the urethra. The body responds by making the bladder walls thicker, but over time, the bladder weakens, leading to incontinence and frequent urination, particularly at night.
Though the symptoms may overlap, the underlying causes and treatments are different. This is why proper diagnosis is important for effective treatment.
Q: What is the Difference Between Prostatitis and Prostate Cancer?
Dr. Shafqat answers: While prostatitis and prostate cancer both affect the prostate gland, they’re two different conditions in their causes, symptoms, and risks.
Prostatitis is inflammation of the prostate, which is often due to bacterial infection. But it can develop without any clear reason. It is not cancerous and is possibly to develop in men in the middle age and young age group.
Prostate cancer, on the other hand, happens when the cells in the prostate begin to grow uncontrollably, forming a tumor. Prostate cancer is one of the most common cancers in men and may either develop slowly or quickly.
Key Differences:
Causes:
- Prostatitis can be caused by bacterial infections, urinary tract infections, or stones in the prostate.
- Prostate cancer is developed through genetic changes to result in unlimited cell proliferation.
Symptoms:
- Prostatitis: Painful or uncomfortable urination, frequent urination, pelvic discomfort, discomfort on ejaculation, and sometimes fever.
- Prostate cancer: No indication in early stages. Later, it can cause urinary difficulties, blood in urine or semen, erectile dysfunction, bone pain, or unexplained weight loss.
Severity:
- Prostatitis is not life-threatening and is usually treated by prescribing antibiotics or other medications.
- Prostate cancer can be very serious, especially if it spreads beyond the prostate.
Treatment:
- Prostatic treatment depends on the cause and may include antibiotics, analgesics, or lifestyle changes.
- The treatment for prostate cancer is graded according to seriousness and goes anywhere from active monitoring, to surgery, radiotherapy, or hormonal treatment.
Q: Does Prostatitis Increase the Risk of Prostate Cancer?
Dr. Shafqat answers: As the research indicates, the relationship between prostatitis and prostate cancer is complex and appears to vary based on the type of prostatitis:
- Clinical Prostatitis: This refers to cases where symptoms are present. Some doctors believe that a history of clinical prostatitis could increase the risk of developing prostate cancer.
- Histological Prostatitis: This type involves prostate inflammation observed under the microscope without any overt symptoms. Interestingly, studies have shown that histological prostatitis is 4-5 times more common in men without prostate cancer than in those with it.
Research findings have varied. For example, one study noted that while the overall history of clinical prostatitis did not significantly raise prostate cancer risk, subgroup analysis revealed that in white males the risk was slightly elevated (though not statistically significant), whereas in African American men with chronic prostatitis, the risk was significantly decreased. Additionally, recurrent or chronic prostatitis, particularly in individuals with a family history of prostate cancer, might increase the risk due to the role of inflammation in fostering cancer cell growth.
Q: Does Prostatitis Go Away on Its Own?
Dr. Shafqat answers: CPPS is a type of prostatitis that sometimes responds to lifestyle changes and may resolve on its own without antibiotics. In any case, the potential for self-resolution largely depends on the underlying cause and the actions taken. Let me explain this in detail:
If you take antibiotics, they might eliminate the specific bacteria causing your prostatitis, but they also affect the entire microbiome in your urinary tract. Current statistics show that even one dose of antibiotics can kill 50% of the beneficial probiotics in your gut. This creates a challenging situation – do you take the antibiotic or not?
One approach I often recommend is to focus on improving your microbiome through:
- Probiotics
- Fermented foods like kefir milk (the most effective option)
- Homemade sauerkraut
- Yogurt
- Kimchee
- Miso
- Kombucha tea
Another effective supplementary treatment can be colonic hydrotherapy sessions. These sessions can help “wash out” waste matter overgrowth in the colon and rectum, creating a better environment for beneficial probiotics to grow and protect your prostate. We’ve seen cases where men’s symptoms of both BPH and prostatitis improved rapidly with colonics or colon cleanses. The Kellogg Clinic has even reported complete resolution of BPH with colonic treatments.
Q: How to Treat Prostatitis?
Dr. Shafqat answers: Treatment for prostatitis depends on the specific type:
Acute Bacterial Prostatitis
- Antibiotics: As the research shows, the primary treatment is a course of antibiotics lasting typically 4–6 weeks.
- Intravenous Antibiotics: In severe cases, IV antibiotics may be administered for a faster effect.
- Urinary Retention Management: If acute urinary retention occurs, a catheter is used to drain the bladder.
- Note: It is critical to complete the full antibiotic course to prevent recurrence and drug resistance.
Chronic Bacterial Prostatitis
- Extended Antibiotic Therapy: Study shows that, treatment usually involves antibiotics for at least 4–6 weeks, with follow-up urine tests to ensure the infection is cleared.
- Recurrent Infections: If symptoms reappear, additional and prolonged courses of antibiotics may be necessary.
- Antibiotic Characteristics: Effective antibiotics for this condition are highly lipid-soluble, have a small molecular size, and low protein binding to penetrate the prostate tissue efficiently.
Chronic Non-bacterial Prostatitis (CP/CPPS)
- Symptomatic Treatment: Since antibiotics aren’t effective here, treatment focuses on symptom relief using medications such as alpha-blockers, 5-alpha reductase inhibitors, and pain relievers.
- Additional Therapies: Studies report that physiotherapy, prostate massage, and counseling for stress and anxiety can sometimes be effective therapies, depending on the underlying cause.
- Rare Cases: In extreme cases, surgery may be considered.
Asymptomatic Prostatitis
- Observation: Typically, no treatment is needed unless laboratory tests (e.g., high PSA or elevated white blood cells in urine or semen) indicate otherwise.
- Antibiotics: In cases with abnormal lab values, a short course of antibiotics (usually 4–6 weeks) might be prescribed.
Q: What’s your perspective on antibiotics for prostatitis?
Dr. Shafqat answers: Prostatitis and antibiotics is a topic that needs careful consideration. While antibiotics are the standard treatment for bacterial prostatitis, there’s growing concern about their overuse. Some interesting studies have shown excessive antibiotic use in men with prostatitis, particularly in non-bacterial cases where they’re not effective.
As such, their use should be limited to individuals with confirmed positive cultures on expressed prostatic fluid or associated urinary tract infection. As research shows, this is because excessive antibiotic use can lead to antibiotic resistance.
The American Journal of Medicine published a study showing that antibiotics were prescribed in 69% of men with chronic pelvic pain syndrome, despite evidence that they’re not effective for this condition. This highlights the need for more targeted antibiotic use.
But what antibiotics treat prostatitis? Common antibiotics prescribed include:
We also sometimes use alpha-blocking agents like tamsulosin (Flomax) to reduce urinary symptoms.
Q: What are the potential side effects of these treatments?
Dr. Shafqat answers: Patients should be aware of several potential side effects:
From alpha-blockers:
- Blurred vision
- Dizziness, drowsiness, and falls
- Headache, chest pain and back pain
- Nausea, diarrhea
- Fever, chills and flu symptoms
Regarding antibiotics, I’m particularly cautious about fluoroquinolone drugs, which carry an FDA black box warning. Misuse of this treatment in susceptible populations can cause severe tendon damage and permanent peripheral neuropathy – causing tingling, numbness, pain, and weakness.
Another concern is the impact on gut health. Antibiotics can destroy beneficial gut bacteria, which are important for your immune system function.
Q: What Natural Treatments Are Available for Prostatitis?
Dr. Shafqat answers: There are several effective natural approaches to managing prostatitis. Let me break down each option:
Diet
Nutrition: Emphasize fruits and vegetables for their vital nutrients, vitamins, and minerals. Also, drink 1.5 to 2 liters of water daily while avoiding coffee, alcohol, and sodas that can inflame the urinary tract.
Food Diary: Some foods, especially spicy foods and citrus, may trigger prostatitis flare-ups. Keeping a food diary can help identify potential irritants.
Dietary Study: An analysis of 2,385 patients (1,710 men and 675 women) with prostatitis/urethral syndrome followed a strict diet eliminating caffeine, alcohol, and hot/spicy foods for 12 weeks, with success rates of 87% in men and 89% in women.

Exercise
Being active helps to maintain a healthy weight, which benefits your overall health. Aerobic exercises, in particular, can relieve prostatitis symptoms.
Italian researchers randomly assigned 231 men with prostatitis to do exercises three times a week for 18 weeks. One group participated in aerobic exercise, and the other group did non-aerobic exercise.
Posture: Following this, it is a good idea to avoid prolonged sitting. Sitting for long periods can put pressure on the prostate gland, eventually leading to inflammation over time. If you are wondering can cycling cause prostatitis, you should know that sitting on a bike seat can have a similar effect, so limiting cycling is also a good idea.
Aerobic Exercise: Regular aerobic exercise has been shown to significantly improve pain levels, anxiety, and depression in men with CP/CPPS.
Pelvic Floor Exercises: Strengthening pelvic floor muscles may benefit urinary symptoms, as pelvic tension is responsible for pain in approximately 50% of CP/CPPS cases.

Probiotics
Supplementation: Probiotics can restore healthy bacteria diminished by antibiotic use. A study demonstrated that men receiving lactobacillus supplements alongside antibiotics had a significantly lower recurrence of UTIs compared to those on antibiotics alone.
Curcumin
Anti-inflammatory Effects: Curcumin, the active ingredient in turmeric, is known for its potent anti-inflammatory properties and excellent safety profile. While its effects on prostatitis alone require further study, the available studies show that it can be beneficial when combined with other natural anti-inflammatories.
Quercetin
- Clinical Evidence: A human clinical trial showed that 1 gram of quercetin daily for four weeks significantly improved symptoms of chronic non-bacterial prostatitis. Further research showed that It may be used alone at a high dose or combined with curcumin and saw palmetto for enhanced effect.

Pollen Extract
- Symptom Relief: In clinical studies, pollen extract has demonstrated anti-inflammatory properties that helped improve symptoms and quality of life in men with chronic non-bacterial prostatitis.
Saw Palmetto
Dual Action: Known primarily as a treatment for prostate enlargement due to its ability to reduce DHT, saw palmetto, as the study shows, also has potent anti-inflammatory effects that may help alleviate prostatitis symptoms.
Prostate Healer
We formulated Prostate Healer to combat BPH and prostatitis effectively and provide symptomatic relief from urgency, frequency, and nocturia.
It works on the prostate, kidney, and bladder simultaneously, coaxing cells gently to resume normal function. So, by this action, you’re fighting against prostatitis and BPH.
If you’re like many men who use the formula, you’ll see a reduction in the number of times you get up to go to the bathroom to urinate. Plus, with our prostate supplements, you’ll see an improvement in the flow of your urine.

Key FAQs on How to Cure Prostatitis
Q: How long does prostatitis last?
Dr. Shafqat answers:The duration of prostatitis will be dependent on the type. Most acute bacterial prostatitis will be sudden and will get better within 24-48 hours if it is treated promptly. Chronic bacterial prostatitis will persist for weeks and sometimes long-course antibiotics will be necessitated. Chronic nonbacterial prostatitis also known as chronic pelvic pain syndrome (CPPS) will persist for weeks to years and will experience intermittent episodes of symptom onset and resolution. The treatment involves symptom management and lifestyle modification.
Q: Can a woman get an infection from a man with prostatitis? Is prostatitis contagious?
Dr. Shafqat answers: Prostatitis itself is not a sexually transmitted infection and is not contagious normally. However if the underlying cause of the prostatitis is an STD like chlamydia or gonorrhea, it becomes a risk of passing the disease to a sex partner. The non-bacterial type of prostatitis does not get passed during sex. Safe sex and getting both partners tested can help prevent any STI-related risks.
Q: Can prostatitis cause ED (erectile dysfunction)?
Dr. Shafqat answers: Yes, prostatitis does cause erectile dysfunction. The inflammation and pain within the prostate might interfere with the nerves and flow of blood and therefore with the erection and the maintenance of an erection. Chronic prostatitis also induces anxiety and stress that might further enhance ED. The treatment of the underlying inflammation and the management of anxiety and stress can alleviate the symptoms.
Q: Can prostatitis cause constipation?
Dr. Shafqat answers: Yes, prostatitis also sometimes results in constipation. The inflamed prostate will at times press against the rectum, causing discomfort and difficulty with bowel movements. Spasming of the muscles of the pelvis and pain also cause constipation. The constipation will at times be relieved with fluids and a high-fiber diet and with the use of stool softeners if required.
Q: Can ejaculating help prostatitis?
Dr. Shafqat answers: Ejaculation may ease the pain of some men with prostatitis by draining the prostate fluid and clearing congestion. Ejaculation might also make the pain worse in a few instances if the inflammation has been acute. The effect will be different with each individual, and it will be wise to take a doctor’s recommendation and observe how the body reacts.
Q: Can prostatitis cause back pain?
Dr. Shafqat answers: Yes, prostatitis can cause lower back pain, particularly in chronic instances. The prostate gland lies near the lower backbone and inflammation will sometimes radiate pain to the lower back, pelvis, or hip area. The underlying prostatitis needs to be treated and pain management techniques such as the use of warm baths and relaxation exercises of the muscles of the pelvic floor will also be useful.
Q: Can kidney stones cause prostatitis?
Dr. Shafqat answers: Kidney stones don’t really cause prostatitis, although they may be a cause of urinary tract infections (UTIs) or urinary retention and potentially an indirect risk factor for bacterial prostatitis. If you’re having a problem with kidney stones and also frequent episodes of prostatitis, removing the stones and easing the flow of urine may help reduce the risk of infection.
Q: Does vaping cause prostatitis?
Dr. Shafqat answers: There is no clear evidence that vaping leads to prostatitis. Nevertheless, inflammation and a change in the immune system that results from vaping might exacerbate the symptoms of chronic prostatitis in men. Poor circulation and elevated oxidative stress that result from smoking and vaping also play a part in affecting the prostate. Eliminating and reducing the use of vaping might enhance the general functioning of the prostate.
Q: What’s Your Concluding Advice for Men Dealing with Prostatitis?
Dr. Shafqat answers:While prostatitis isn’t life-threatening, it can significantly impact quality of life. I recommend a holistic approach:
- For bacterial prostatitis, probiotics are essential
- A combination of saw palmetto, curcumin, and quercetin has proven clinically effective for pain reduction
- These natural supplements can also help prevent unnecessary PSA tests by reducing inflammation and PSA levels.
Now that you know what prostatitis is, remember the key is taking a comprehensive approach that benefits not just your prostate but your entire body.
Our Medical Review Process
At Ben’s Natural Health, we prioritize transparency, accuracy, and scientific integrity. Every piece of content is carefully developed by medical professionals and undergoes a thorough review every 12 to 24 months. This rigorous process ensures our information remains current, evidence-based, and trustworthy. We exclusively reference peer-reviewed studies from reputable medical journals, providing full citations and direct links to maintain credibility. Learn more about our medical review process and research standards.
Our Editorial Guidelines
For over 25 years, Ben’s Natural Health has been a trusted source of scientifically accurate information on natural health. Our editorial guidelines uphold the highest standards of quality and integrity. Each article is written by qualified professionals—including doctors, dietitians, nutritionists, fitness experts, and surgeons—and undergoes independent quality checks. We emphasize transparency by clearly displaying the credentials and biographies of our contributors at the beginning of every article. Read our editorial guidelines to understand how we create and fact-check our content.
Medical Disclaimer
The content on this blog is for informational purposes only and should not be considered a substitute for professional medical advice, diagnosis, or treatment. While our articles are reviewed and authored by licensed medical professionals, they may not address your specific health concerns. Always consult your primary care physician or a qualified healthcare provider before making any health-related decisions. Never ignore or delay seeking professional medical advice based on the information provided here. Your use of this blog and its content is entirely at your own risk.